Guided Bone Regeneration (GBR) has been one of the most common surgical procedures in Implantology for the last decades.
As new regenerative treatments are developed, GBR still remains the most performed procedure among the surgeons to gain bone for proper implant placement and long term stability.
Guided Bone Regeneration would be consider the gold standard technique since it adapts to any scenario and can be performed by any clinician with certain experience.
The question resides on which are the factors that will determine a successful treatment?
Some of the most important will be described here and one of the most detrimental is membrane fixation.
Which are the most important factors for proper Guided Bone Regeneration?
1-. Patient selection: The patient needs to be a candidate for that specific treatment, so smokers, deficient OH, non controlled diabetes and other genetic factors would alter the results and we must consider them at the time of performing the surgery.
2-. Good soft tissue quality: Commonly the lack of sufficient bone is followed by lack of KG (watch Soft Tissue Mastercourse) for proper surgical closure and enough KG around our implants.
3-. Anatomical Knowledge: Correct Interpretation of CBCT is mandatory to avoid damaging any important area such as lingual concavity at lower mandible, IAN, maxillary sinus etc…
4-. Incision design that requires vertical releasing incisions away from adjacent teeth and surgical site and Periosteal release for no tension and primary closure.
5-. Biomaterial selection: Read article 5 important Biomaterials in Regenerative Surgery to find out the different properties for each case and vital bone turn over for predictable results.
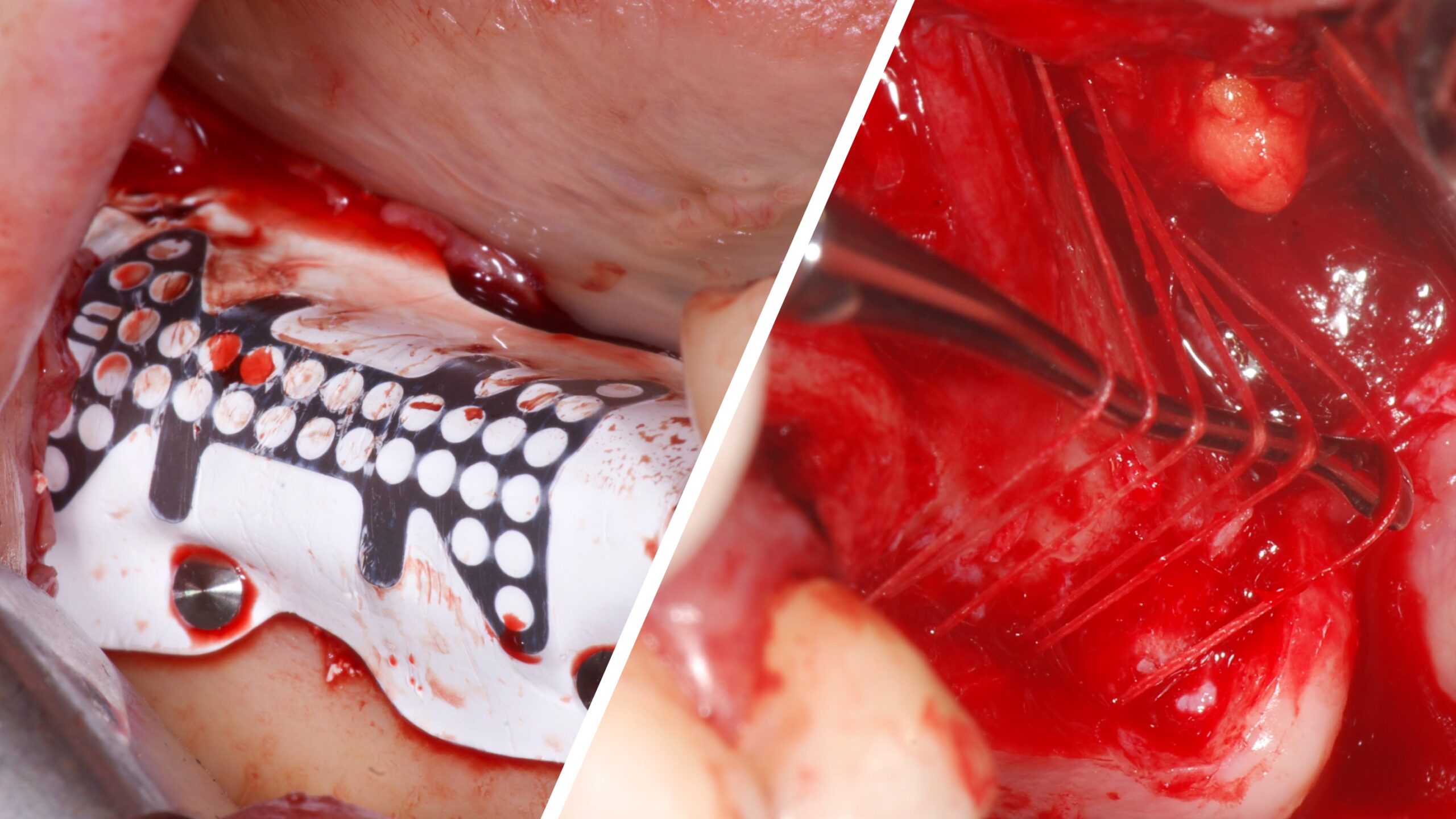
6-. Membrane selection and Fixation: A non fixed and very quick resorbable membrane will not avoid soft tissue migration and particle encapsulation so Pericardium membranes are more stable, rigid and have a very slow resorption process as long as we stabilize them in moderate cases.
Severe cases would require a non resorbable PTEF membranes Ti Reinforced or titanium membranes to recreate the original volume lost.
Depending on the location, the size of defect and the type of defect the membranes should be fixed and stabilized by different mechanisms either tacks or periosteal sutures. Which are the advantages and disadvantages of one or the other?
Tacks:
Advantages:
- Quick and easy to use.
- They can be kept if not recovered in second stage (titanium made)
- You can hammer them or shoot them with specific device (Bio-Horizon Auto Tack)
- Easy to remove.
Disadvantages:
- They need a perpendicular position for predictable insertion.
- With Hard cortical plate there is a risk of fracture the tack.
- Not cheap, especially the good ones.
- Lingual placement and Palatal position are difficult to insert.
Sutures:
Advantages:
- The fixation is well distributed along the membrane not only at the edge sites. It provides with membrane compression and good stability over the graft.
- It can be performed at any location with no limitations.
- Very cheap since they are resorbable sutures.
- They don’t need to be removed.
Disadvantages:
- Needs a training for predictable outcomes. Watch Free Masterclass IMMEDIATE IMPLANT AND GBR IN THE AESTHETIC ZONE.
- It takes a longer time to perform than tacking.
- It requires good visibility for periosteum anchorage. Loupes with led light vision are recommended.
Additional factors for GBR such as Khoury technique by the use of autogenous cortical bone harvested from the ramus and new hosting bone frame, screw tenting technique for space maintenance are some of the “enhancements” of this technique which keeps the essence of hosting the particulate bone inside of a closed environment.

Great
Thank you very much
Thank you. What type of sutures you recommend to fix membrane?